Activity-based costing in the OR
Value-based healthcare is transforming the way healthcare systems measure performance.1 To successfully implement value-based healthcare, hospitals must find a way to effectively determine the cost for each patient’s care. Activity-based costing (ABC) is one such method that has gained prominence as more hospitals turn towards using this model to gain a better understanding of their financial performance
What is activity-based costing and why is it needed?
Activity-based costing calculates cost based on resource usage, a bottom-up approach that makes isolating OR costs simpler than the typical top-down approach frequently used in hospitals.
Top-down approaches use defined metrics to evaluate a total cost by a group of activities whereas a bottom-up approach aggregates the cost to each resource used, breaking it down by activity.
Although most hospitals are aware that surgical costs are the largest contributor to hospital costs, this model allows for the financial performance of the OR to be assessed directly.
Get better insights to improve financial performance
Surgeons too, are increasingly finding themselves in the driving seat to improve efficiency to help enhance the OR’s financial performance.
Traditional top-down approaches to costing provide little insight to surgeons and surgical staff on where to focus their efforts. But with activity-based costing, it is possible to not only identify opportunities for cost reduction but also to predict the impact of any efficiency improvement measure.
Further to that, once improvement measures have been implemented, activity-based models are a great tool to evaluate the impact of any changes over time on the overall financial performance of the OR.
Maybe you’re also interested in: Introducing Efficiency for the Direct Anterior Approach Surgery with Prof. Dr. Corten.
Benchmark against the market and other hospitals
It can also be a very helpful exercise to benchmark the financial performance of the OR against the market or other hospitals, say within a health system, to identify which ORs can perform better.
Benchmarking is better enabled by the bottom-up approach as it provides a more accurate financial impression of the OR performance as opposed to the traditionally used relative value units or ratios of cost to charges.2
Create a business case to justify investments
The shift towards value-based healthcare has made improving OR efficiency critical to ensure costs are reduced while maintaining great quality of care.
To that end, investment in change, be it new technologies, medical devices, or processes, can be supported by making an accurate business case further supporting value-based purchasing.
Although the value added with activity-based costing is clear, it is not utilized enough in healthcare because of the difficulties posed by data integration and access from the variety of different systems storing and dealing with data. This is where DEO comes in with our data insights and analytics platform.
How do we use activity-based costing to assess the OR?
DEO’s AI-backed data insights and analytics platform captures more than 50 data points in the OR per case including the timing of specific activities, costs, and the general OR set-up with respect to resources, material, and process flow.
Timestamp measurements are used to determine the timing of specific activities in the OR process. These timings add up to the overall procedure time and influence both the cost of a procedure as well as the OR throughput.
Material and resource usage information along with their associated costs determine the cost per procedure in our financial model.
Fixed costs account for costs that are incurred daily, irrespective of whether one or ten surgeries take place. When more surgeries can be done in one day, the fixed cost of each procedure is less.
Variable costs, on the other hand, are fees linked to a specific procedure and occur with every case performed. To reduce these costs, material and resources must be optimized.
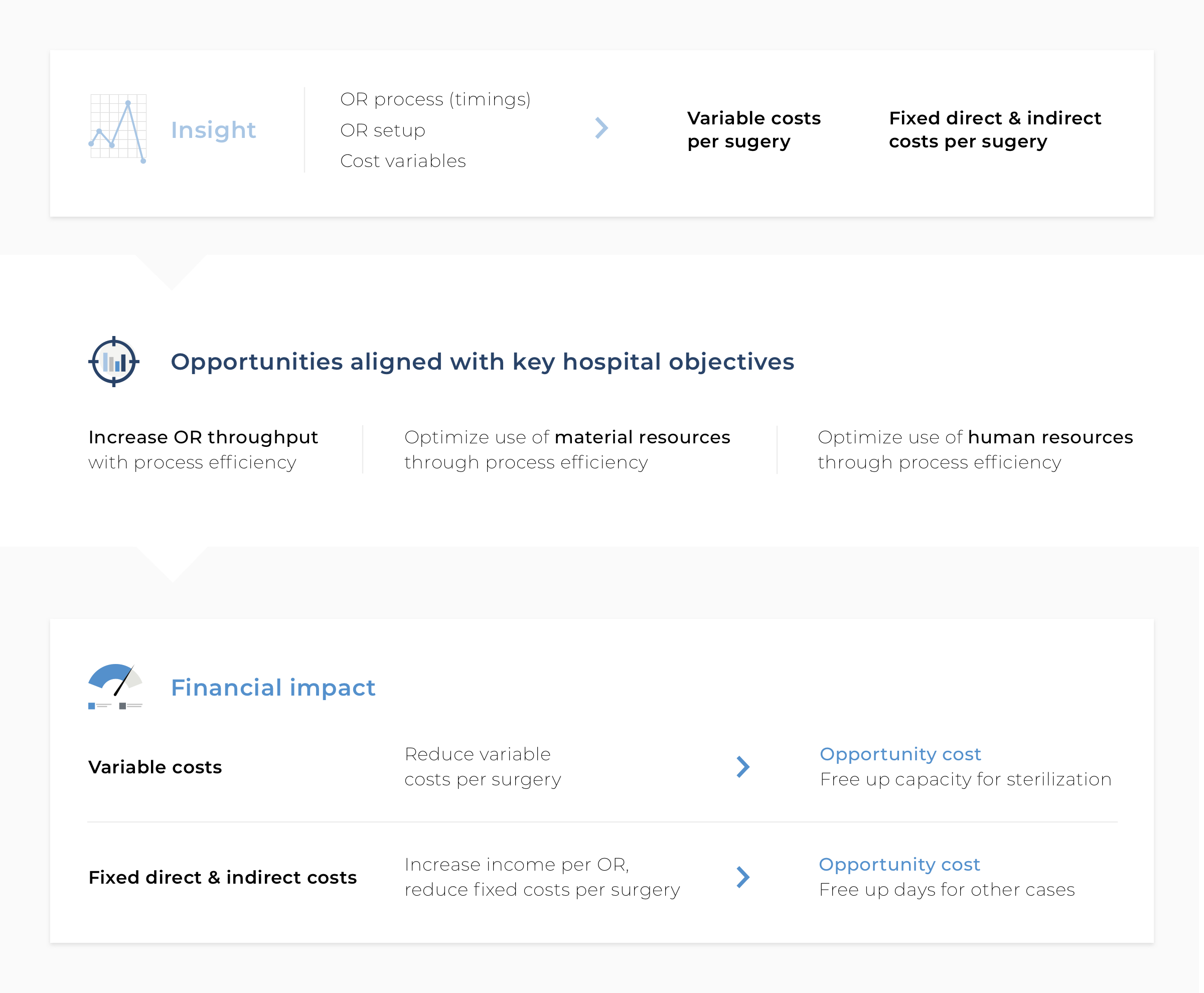
All this information is measured in our data analytics platform over a dedicated observation period and is fed into our automated financial performance calculator which uses a parameterized model to provide a unit cost per procedure.
For DEO this is a simple and straightforward process allowing the hospital a quick assessment of their OR’s financial health.
Although all this data is accessible to the hospital, the lack of visibility between various systems makes the process of putting everything together cumbersome without the help of a platform like DEO.
Financial model in action
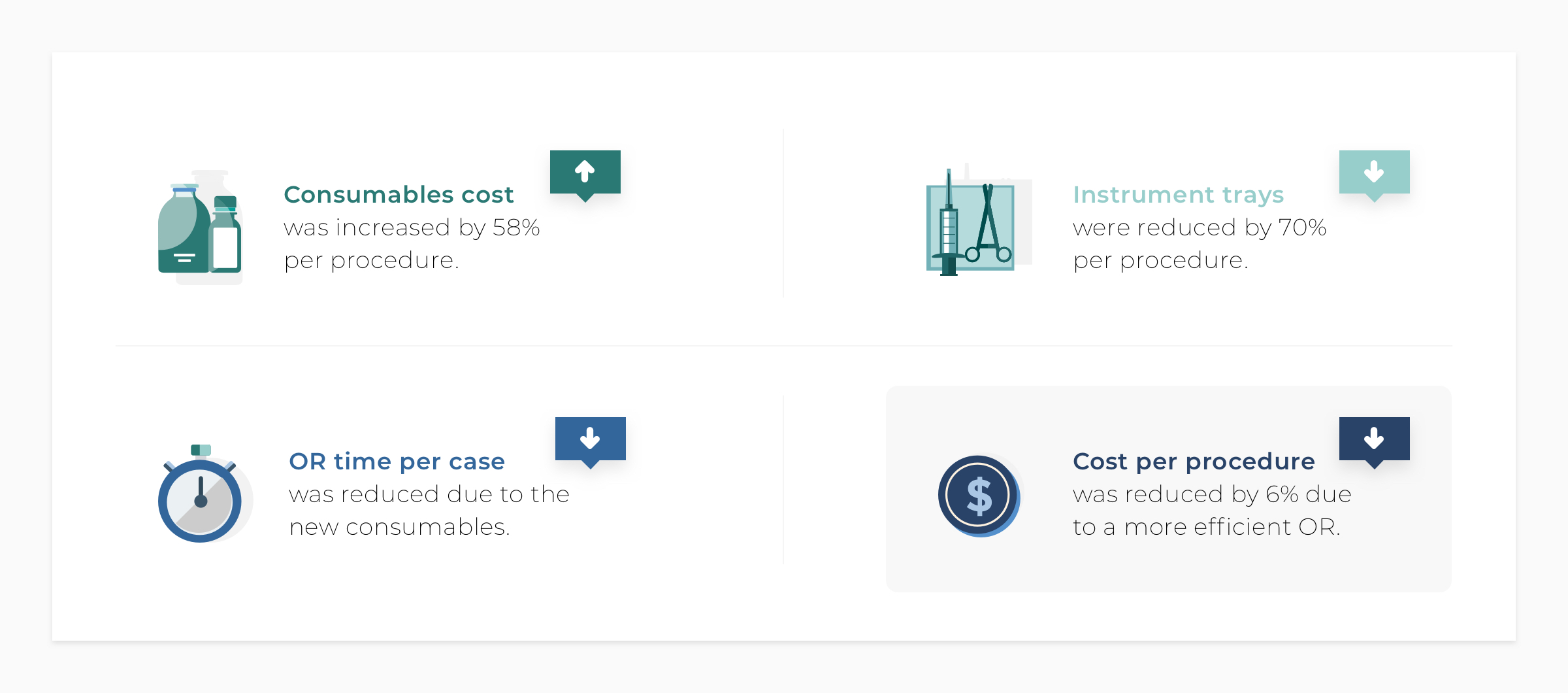
A partner hospital was interested in purchasing items that the surgical team believed would improve OR efficiency, but which would increase their consumables cost by 58% per procedure.
As it turned out, DEO’s measurements confirmed that these new consumables facilitated a reduction in OR time for each case, as envisaged by the surgical team. Alongside purchasing the new consumables, the hospital also implemented a 70% reduction in instrument trays used per surgery. This result was a more efficient OR process, so much so that the overall financial impact was a reduction in cost per surgery of 6%.
At a macro level, DEO’s activity-based cost model projected an overall annual cost saving for the hospital of 8%. In addition to these cost savings, the simulation also demonstrated the opportunity for additional income thanks to freeing up 59% more OR days per year.
By using an activity-based cost model, the various activities impacting the cost of a procedure are directly visible, making it easier to spot opportunities and limit risk. The transparency that this provides stakeholders enables an objective perspective—a view that is necessary when it comes to implementing value-based healthcare well.
Do you want to know how we can help you get started? Schedule a 15-minute intro call. No strings attached.
PS. If you enjoy this content, you will definitely love the stuff we share on LinkedIn. Make sure you stay in the loop and follow our LinkedIn page.
Footnotes
- Mjåset, C., Ikram, U., Nagra, N. and Feeley, T., 2020. Value-Based Health Care in Four Different Health Care Systems | Catalyst non-issue content. [online] Catalyst.nejm.org. Available at: <https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0530>
- Najjar, P., Strickland, M. and Kaplan, R., 2017. Time-Driven Activity-Based Costing for Surgical Episodes. JAMA Surgery, 152(1), p.96
Add Comment
You must be logged in to post a comment.