Operational excellence performance metrics
Operating rooms (ORs) are commonly referred to as the heart of any surgical hospital and impact most, if not all, other organs of a well-functioning hospital.
In financial terms, the OR is the largest revenue generator for the hospital. But, at the same time, the OR is also the most significant cost driver in perioperative care and accounts for about 30% of the total cost, covering equipment, staff, facilities, consumables, and so much more.
As such, it should be no surprise why there’s a big focus on managing ORs efficiently at many hospitals seeing that ORs ultimately can determine the financial viability of a healthcare organization.
But what operating room efficiency metrics matter to measure how well an organization is doing?
In this guide, you’ll learn:
- Which operating room efficiency metrics to look at.
- How to measure these metrics.
- What standards you can use to compare performance.
This guide is three-fold and comes in three parts, with the first one predominantly covering metrics on process efficiency. Future chapters will explore insights on well-being and ergonomics and financial performance
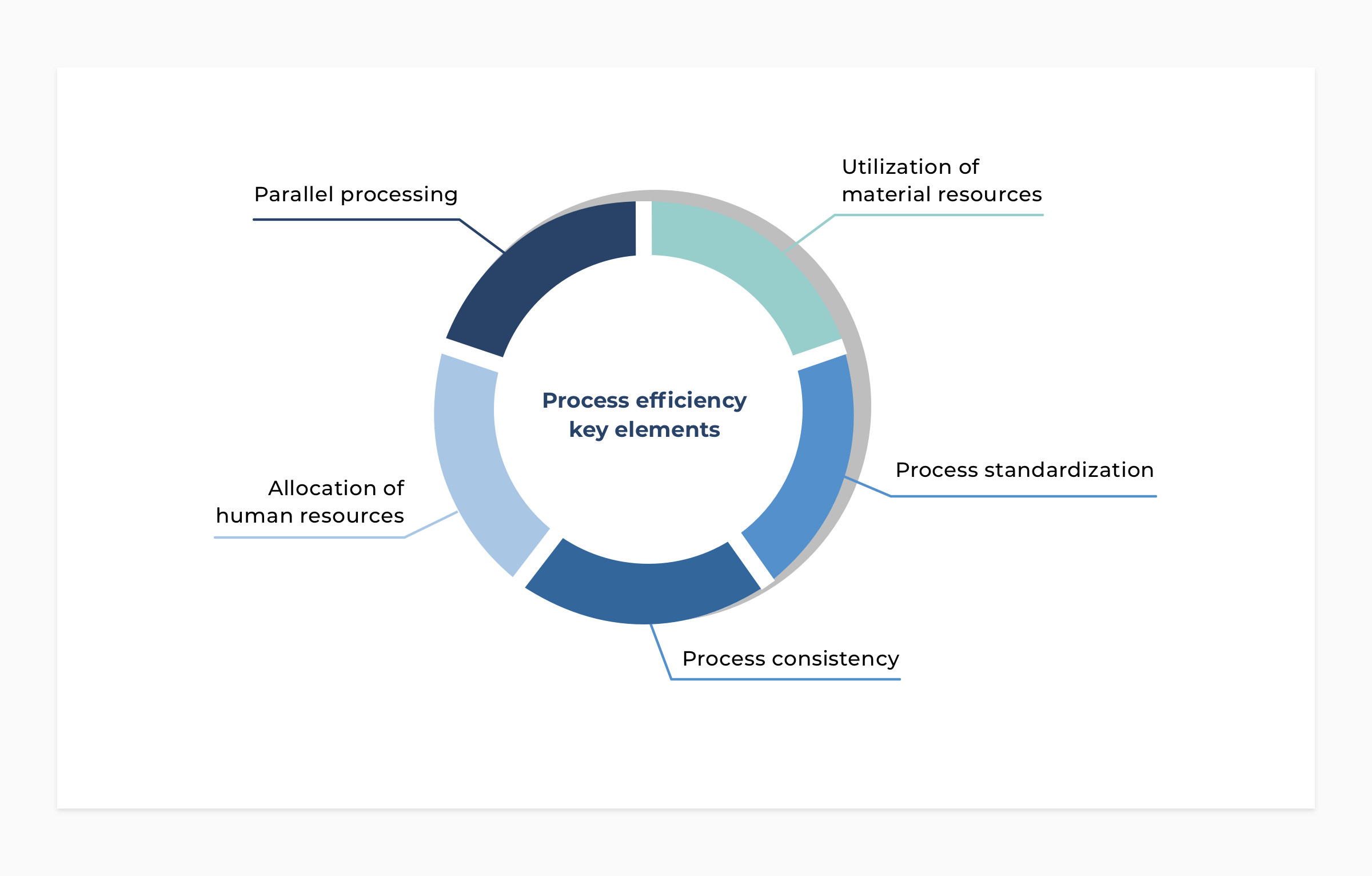
5 key elements of process efficiency
Process efficiency is an excellent measure to quantify the efficiency of specific processes in the OR and identify opportunities on how surgical teams optimally can perform a set of tasks to ensure a smooth flow.
This is especially important in high-volume and standardized procedures where outcomes should be reproducible and predictable to consistently maintain the same patient care.
When we look at insights on process efficiency, we consider five elements that are all linked and impact the ability to achieve process efficiency goals.
- Process standardization
- Process consistency
- Parallel processing
- Allocation of human resources
- Utilization of material resources
#1 Process standardization
Essentially, standardization outlines a set of steps for how people must conduct a specific task or several tasks in a flow. It’s about having a plan and following that plan, which has proven to yield great results in healthcare and inside the operating room.
Knowing what to expect in the OR process allows the team to work in concert with the right materials, and following a plan also minimizes fatigue and reduces the risk of human mistakes.
#2 Process consistency
Consistency and standardization are closely linked. Both enable predictability, which is a critical component for optimal surgery scheduling, allocation of resources, and the flow of medical staff.
When we look at consistency in the operating room, it’s a matter of identifying which steps are consistent and which actions or variables cause inconsistencies—whether in the setup or breakdown of the OR or the surgical process. Now, the patient always introduces some variability, and this should naturally be considered. Therefore, variability caused by the patient is an inconsistency that one can try to improve, or an inherent variability to take into account.
#3 Parallel processing
Parallelization of processes implies, for instance, that the material and patient flow are performed in parallel when feasible and fully aligned. Now, some processes must naturally be completed before others can start, while others can run parallel to increase overall process efficiency.
Look at the two examples below.
Example #1: During preparation, the patient and materials are prepared at the same time.
Example #2: Breakdown of the OR can already start for implant-related instruments as soon as the components have been inserted and the surgeon starts closing the wound.
Maybe you’re also interested in: How Dedicated Surgical Teams Improve Efficiency and OR Throughput.
#4 Allocation of human resources
The goal is to make sure all surgical team members, like the surgeon, fellow, nurses, and anesthesiologist are aligned in terms of
- roles,
- tasks,
- timing,
- expectations, and
- responsibilities
to prevent no steps in the process are omitted, avoid chaos, and ensure a smooth of tasks for specific processes.
#5 Utilization of material resources
Utilization of resources focuses on eliminating waste by optimizing resource usage to create a reproducible and cost-effective environment. Here we look at two key areas: human and materials resources.
The team inside and outside the OR is an essential element in the total cost per surgery. At the same time, the team is also the most critical success factor in the surgery execution, and for that reason processes and the environment must be designed in such a way that allows the team to perform optimally.
Example: Through standardization, simplification, and the implementation of new medical devices, Prof. Corten and his team now run two parallel ORs instead of one OR, with the same team.
In this example, optimization of human resources has been one of the contributors to reducing the operating room time and, in turn, increase OR throughput.
Besides the cost of human capital, material resources count, too, and interesting metrics include, for instance, OR utilization, instrument utilization, and consumables.
Operating room efficiency performance metrics
To obtain insights on the five elements above, and identify improvement opportunities, we employ several performance metrics.
Some of the most important performance metrics are listed below, followed by an example to show how we quantify the performance.

Example: performance metrics in action
While data is crucial to obtaining insights into the OR processes, it also gives us an in-depth understanding of the processes surrounding surgery.
Our experience shows that opportunities for improvement are often found in the preparation and breakdown of the operating room.
For instance, after measurements in a partner hospital, data showed variability in the preparation phase. Generally, the goal should be to achieve a low variability (high consistency) for non-surgical phases, like the preparation process.
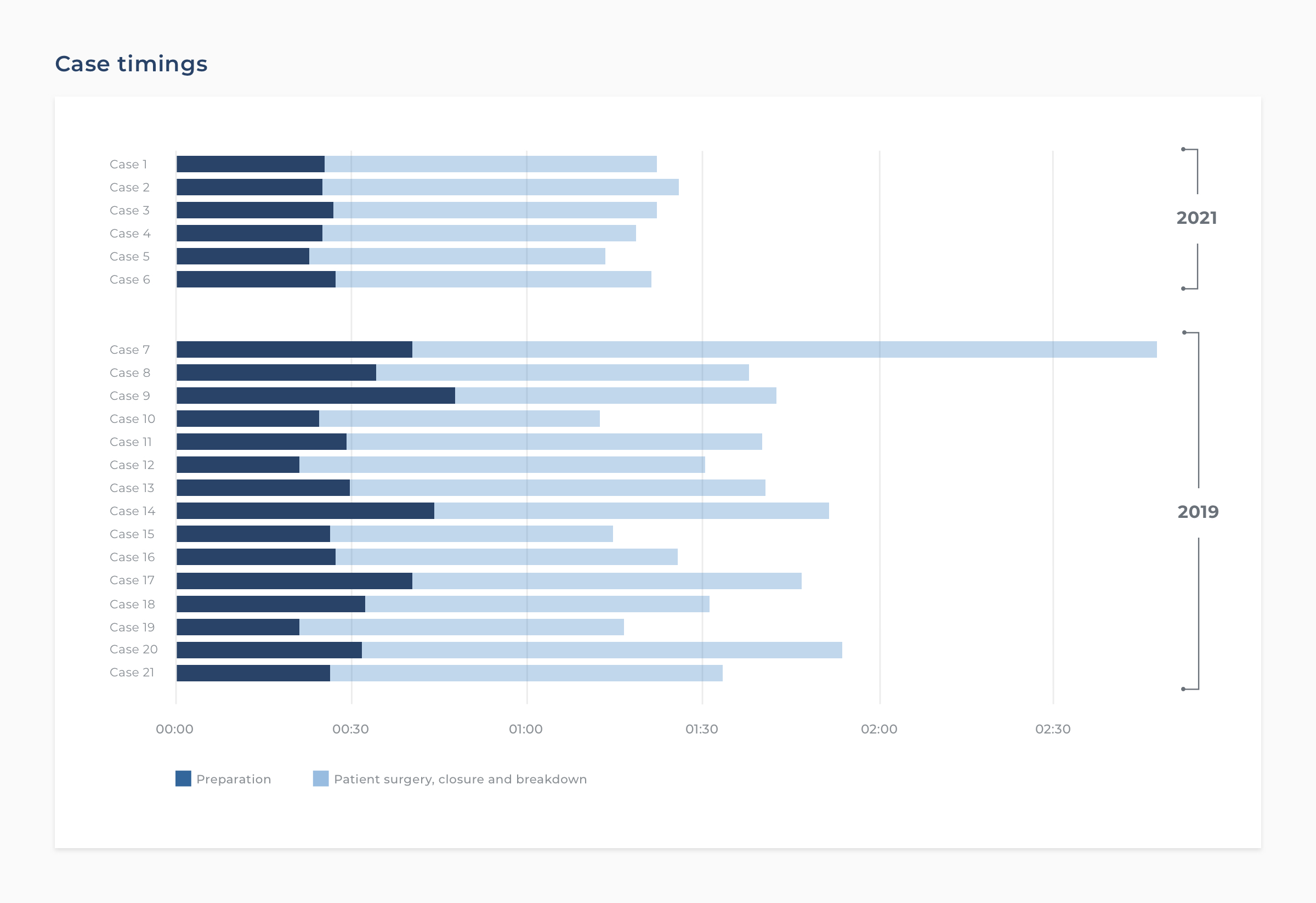
Consequently, the surgeon introduced parallel processing to decrease preparation process variability, aiming to reduce the overall turnaround time.
Previously, the surgeon would wait on the sidelines, scrub, and get into the OR when the patient was ready. Now, he gets into the OR immediately, installs, and starts prepping the patient while other team members handle other activities for the OR preparation.
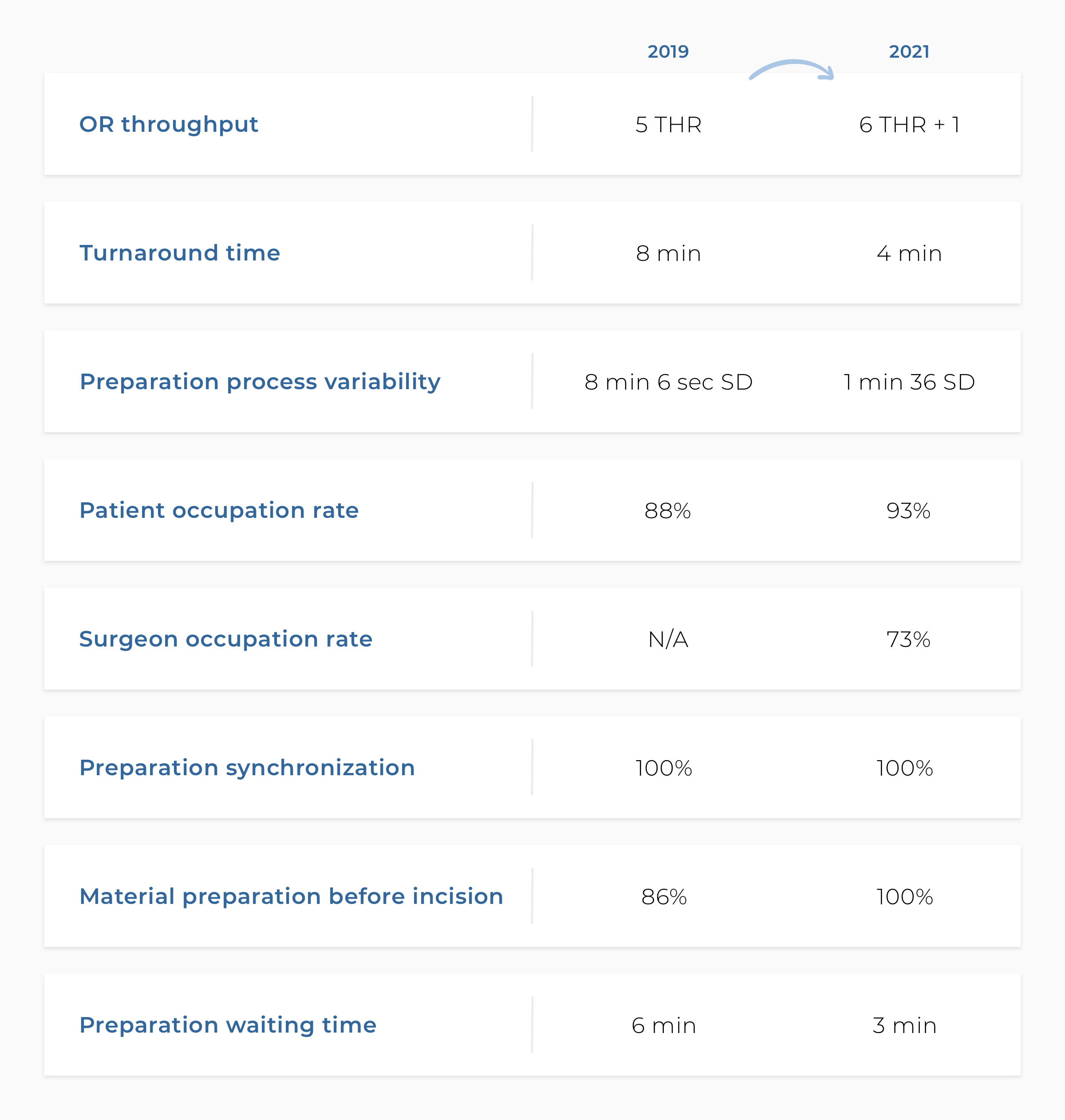
Even what appears to be minor improvements, in this case, has ultimately shown to save the partner hospital a lot of time as shown in the metrics overview below, comparing 2019 and 2021.
Do you want to know how we can help you get started? Schedule a 15-minute intro call. No strings attached.
PS. If you enjoy this content, you will definitely love the stuff we share on LinkedIn. Make sure you stay in the loop and follow our LinkedIn page.
Add Comment
You must be logged in to post a comment.