Professor Corten, Dr. Vanbiervliet, Belgium: Blueprint for a hyperefficient OR for Total Hip Surgery
The demand for total hip arthroplasty (THA) surgery has been rising with the aging population. At the same time, hospitals are facing challenges with surgical backlogs, staff shortages and budget pressure. As a result, there is great incentive for hospitals and surgeons to drive operational excellence initiatives. Increased OR throughput, improved patient experience, optimized financial performance and improved well-being and ergonomics of the surgical team are therefore the key objectives for operational excellence in the efficient OR as discussed by Verhaegen et al. (2022).
The anterior approach for THA allows surgeons to work between the muscles and tissues without the need to release any muscles or tendons from the pelvis or femur. An increasing body of evidence already suggests the anterior approach supports faster recovery, improvements in short term outcomes and reductions in the total cost of care.
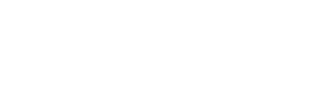
Using the DEO.care platform, real world evidence from 2 orthopedic surgeons has been collected. Dr. Vanbiervliet and Prof. dr. Corten successfully implemented the anterior approach in their OR’s, leading to up to 7 THA procedures a day in 1 OR (dr. Vanbiervliet) and up to 14 THA procedures a day in 2 parallel OR’s (Prof. dr. Corten) with six team members (i.e. surgeon, anesthesiologist, fellow, scrub nurse, circulating nurse and anesthesiology nurse). The figure below shows the OR day and total OR time of both surgeons on average.
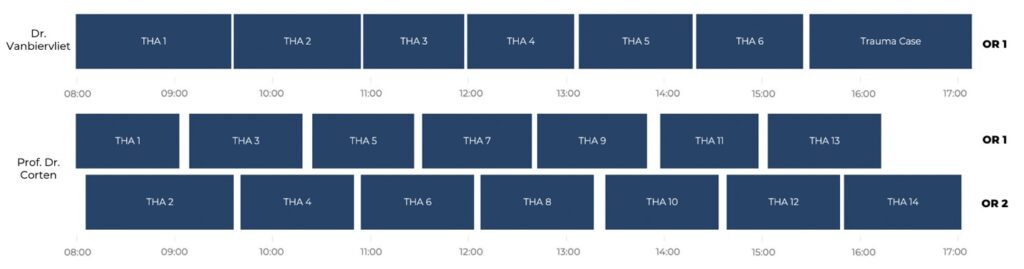
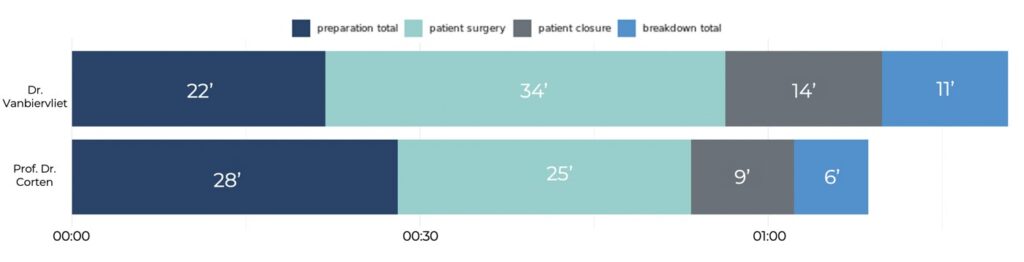
Figure 1: (Top) shows the number of cases laid out across each OR between 8am and 5pm. (Bottom) shows the average time per case for preparation, surgery, closure, and breakdown phases of each case.
Dr. Vanbiervliet and Prof. dr. Corten have implemented the following best practices to achieve operational excellence in their respective operating rooms:
Standardization and consistency
Using the same team, the same materials and the same techniques for every hip replacement procedure has allowed dr. Jens Vanbiervliet and prof. dr. Corten to standardize their procedure and maximize consistency to increase the operational excellence in their OR’s. The graphs below show the standardization of processes for preparation, patient surgery and breakdown of both surgeons.
Figure 2: Process flow for Dr. Vanbiervliet (Top) and Prof. dr. Corten (bottom). Each line in the graph represents one surgery, from preparation to breakdown phase. The closer the lines are to each other the more consistent the process is. Each point represents a timestamp during the process. When the timestamp (points) follows the same order across each line (surgery), this indicates the process is more standardized.
Team optimization
The team of dr. Vanbiervliet and prof. dr. Corten includes a fellow/resident, an anesthesiologist, a scrub nurse, a circulating nurse and an anesthesiology nurse. Surgical team alignment and clarity on roles and responsibilities make it possible to streamline the whole procedure flow.
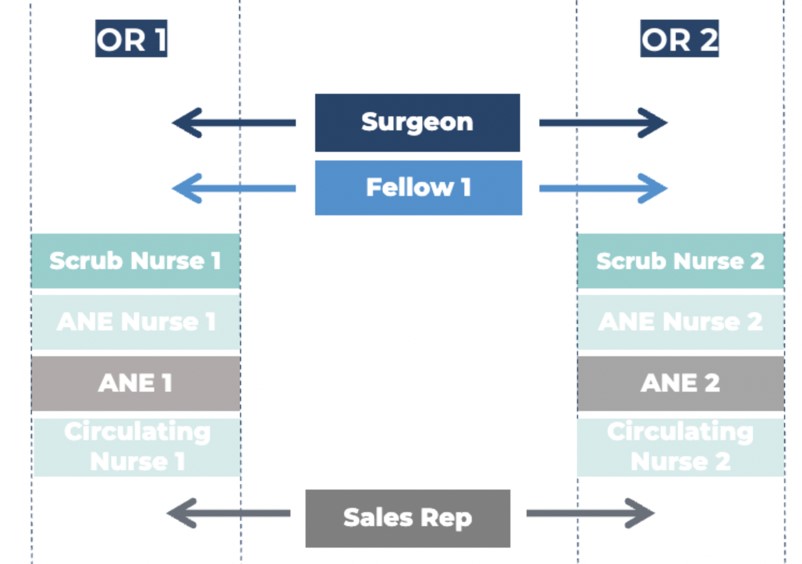
Figure 3: Surgical team allocation of prof. dr. Corten in 2 parallel OR’s.
Anesthesia optimization
New loco-regional anesthesia techniques are used specifically tailored to hip surgery and are performed in the anesthesia ward next to the OR. In this way, the patient is ready to be disinfected and draped for surgery from the moment he enters the OR. Patient preparation and material preparation can be performed as parallel processes, supporting efficient preparation times and consequently reducing the overall OR time.
Optimized instrument trays
The instrument trays are optimized and reduced to just three trays per procedure. Tray reduction not only reduces sterilization and storage costs but can also improve physical wellbeing of the surgical staff since fewer heavy trays need to be carried around. Additionally, less instruments allow more standardization in material table preparation and breakdown which in turn speeds up the overall process and potentially improves mental well-being of the surgical staff.
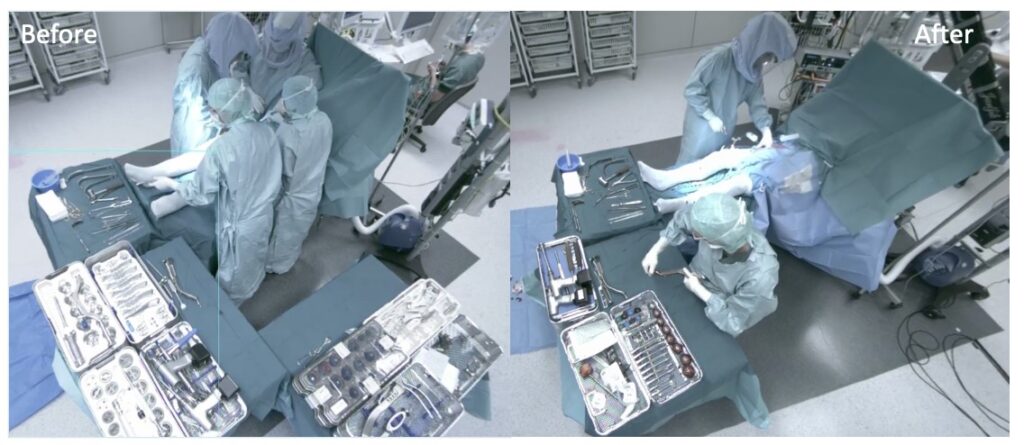
Figure 4: shows a before (left) and after(right) image of the instrument tray set up before and after the optimization of trays was implemented.
Efficient Draping System

The EsySuit® is an efficient, standardized and ergonomic draping system developed to drape the patient in one fluent movement with one single drape. Draping with the EsySuit® doesn’t only have the potential to reduce draping time but also to improve ergonomics and reduce infections.
Handless Retractor Holding
The gripper technique used during the procedure, where 2 GRIPPERS® are connected to the OR table holding retractors, allows the surgeon to control a stable retractor position without extra help of a fellow and/or nursing staff in the sterile environment. This creates the option to re-allocate surgical staff to different activities or run parallel OR’s without doubling the staff. In addition, the use of the grippers reduces post-operative blood loss and post-operative inflammatory response, as mentioned by Opsomer et al. (2020).
Due to the increasing demand for THA on the one hand and the hospitals facing challenges on the other hand, the drive for operational excellence is greater than ever. Parallelization and standardization of patient and materials flows, hyper efficient patient and material preparation, well-trained surgeons and staff, supportive work environments and reduced instrument sets contributes to operational excellence and drives the quadruple aim in the OR. The observed best practices described above are accessible and easy to implement in any OR environment and can be used as an example for other orthopedic centers and hospitals throughout Europe and the US.
References
Verhaegen J., et al. (2022). Perioperative Operating Room Efficiency Can Make Simultaneous Bilateral Total Hip Arthroplasty Cost-effective: A Proposal for a Value-sharing Model. Arthroplasty Today.
Opsomer G.J., et al (2020). Orthostatic retractor placement reduces operating time and post-operative inflammatory response during the learning curve of anterior approach THA. J. Orthop. 22:503-512.