Professor Corten, Belgium: Efficiency for Direct Anterior Hip Surgery
“It will be difficult.”
“I’m worried about how we can maintain quality of care.”
“Efficiency doesn’t belong in the operating room. We can’t risk a trade-off between patient care and cost reduction.”
These were some of the responses Prof. dr. Kristoff Corten, Orthopedic Surgeon at Ziekenhuis Oost-Limburg (ZOL), encountered when he introduced operating room efficiency.
For the past years, we’ve been working together to define the best pathways to transfer his experiences to other operating rooms after fully validating the concept in ZOL.
Today, Prof. Corten shares his experiences of introducing efficiency to his surgical team for Direct Anterior Approach Total Hip Replacement surgery.
“It is all about eliminating process variables,” he starts.
Why operating room efficiency?
“People are not always receptive to the idea of efficiency because there is a tendency to assume that efficiency is equivalent to cost reduction which doesn’t align with high quality of care. But it’s quite the opposite.”
“Eliminating as many operative process variables as possible, allows us to standardize each step of the surgical procedure. The starting point is improving the ergonomics of the OR process in order to amplify the performance of the surgical team. Doing so, we’re able to reduce the mental and physical fatigue of the surgical team and ultimately improve the process outcomes which has a positive impact on quality of care.”
“When it comes to efficiency, less is more, and the numbers show that,” says Prof. Corten and adds, “There is also a significant economic impact to our efficiency measures.”
Maybe you’re also interested in: The Why, What, and How of Operating Room Efficiency.
Henry Ford introduced us to process standardization. Soon, more and more industries have adopted this methodology. Prof Corten has applied the same principle in his operating room by standardizing the OR process for Direct Anterior Hip surgery.
“As Mr. Ford taught us, everything starts with the reduction of process variables in order to improve the ergonomics and improve the performance of the team. Ultimately, this leads to a reduction of adverse outcomes and an improvement of quality of care. This is for me the ultimate example of value-based care,” Prof. Corten says.
It always starts with people
There is one thing we learned from the pandemic: everything starts with the team. The nurses, the doctors, and the cleaning team. Everybody plays a crucial role to achieve the highest quality of performance.
Therefore, a sustainable efficient process must also create a positive and supportive environment for the surgical team. We begin by looking at ergonomics because this directly affects team performance.
- How can we reduce mental fatigue?
- How can we reduce physical fatigue?
Prof. Corten agrees that the ergonomic perspective is sometimes overlooked in terms of process improvements although it is one, if not THE key aspect to a sustainable healthcare sector.
“The team is an absolutely critical asset to delivering safe and efficient surgeries for patients. We should continuously be looking at how we can improve the work conditions so every nurse, anesthesiologist, and surgeon persistently can do the best job possible,” adds Prof. Corten.
How to measure ergonomics
In ZOL, DEO has measured the ErgoScoreTM of the surgical team. The DEO ErgoScoreTM is an ergonomic evaluation and quantification of the fatigue that staff experience during the surgical process flow.
While this ergonomic evaluation in itself doesn’t improve the work conditions for surgical teams, it provides critical insights into what can be improved and what the impact of this improvement will be.
Prof. Corten continues, “The only way to protect our quality of care is by critically evaluating what we do and how we do it. That also means taking good care of our healthcare professionals, so they can, in turn, maintain excellent patient care.”
“By looking at the physical and mental fatigue and improving this, we’re able to conduct the procedure more swiftly, reduce the surgical trauma, reduce the operating room time, and consequently the anesthesia time—all factors that play a part in improving the patient’s recovery. But even more importantly, this reduces the risk of errors and complications.”
Standardization: every procedure should be the same
One huge factor in improving ergonomics is linked to standardization of the surgical process.
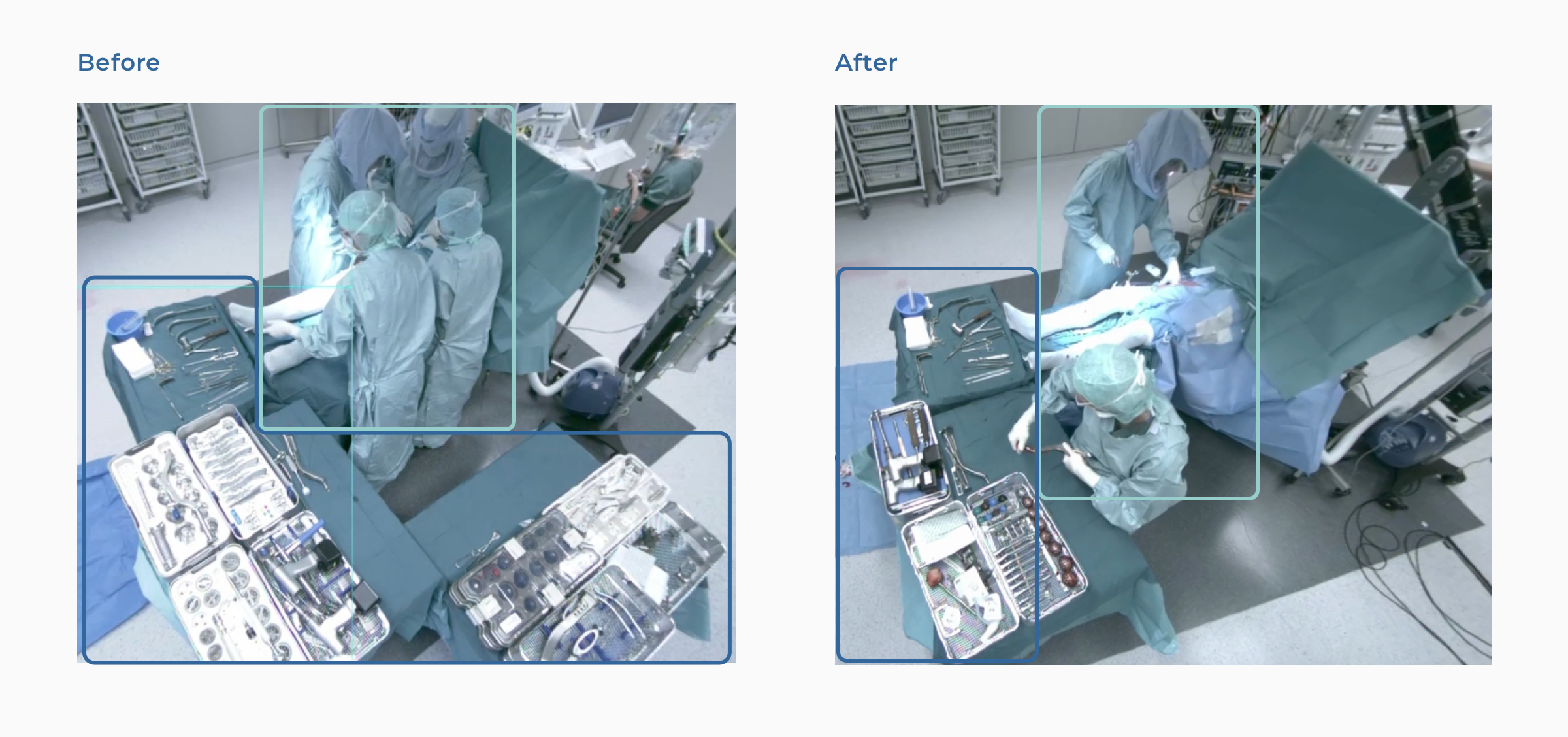
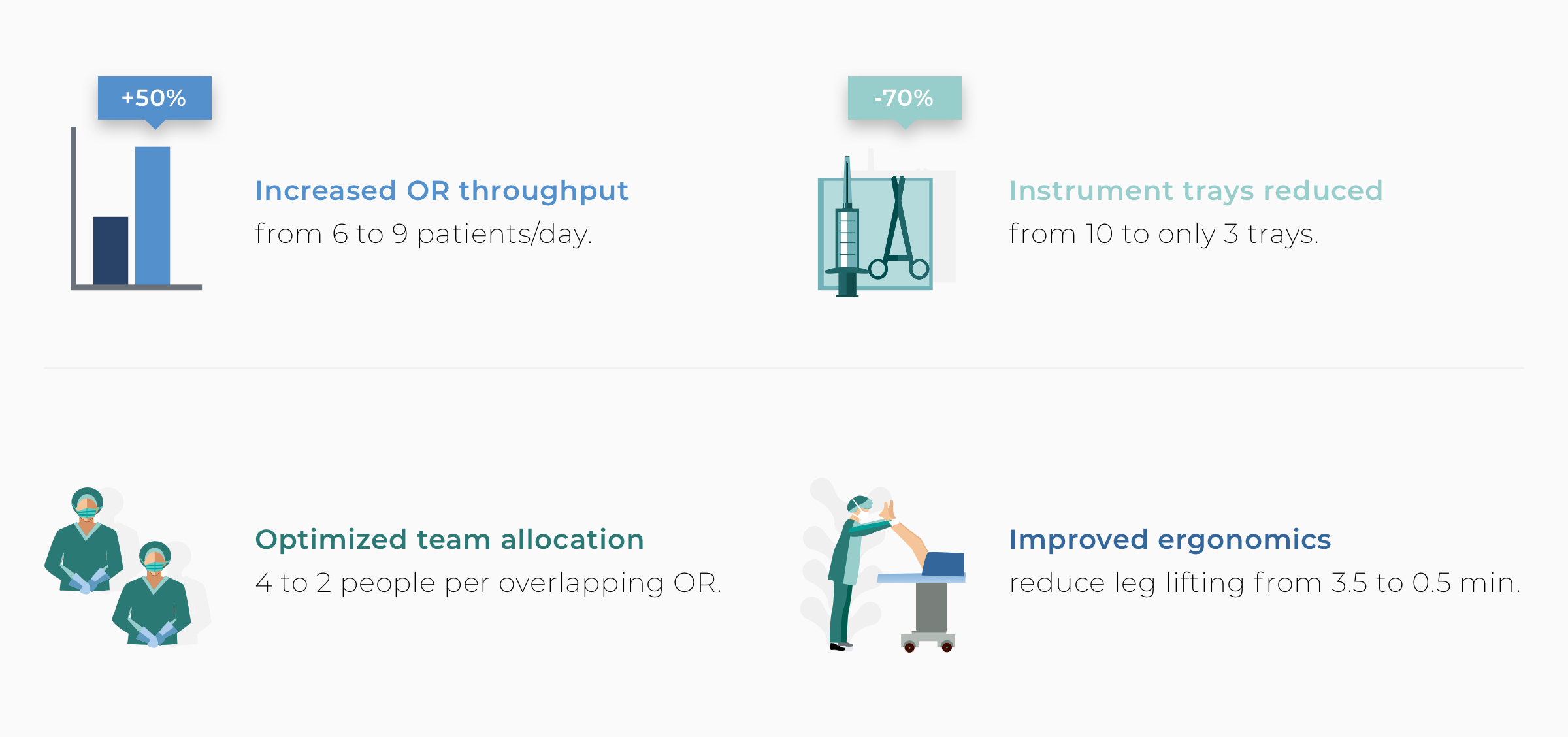
“When I have visitors in my OR, they’re always perplexed at how we can deliver the same procedure with two scrubbed people in the room instead of the four people that used to be there. The answer isn’t secret. It’s all thanks to standardizing the process and thoughtful investment in the right tools,” states Prof. Corten.
He adds, “Now, it’s not that the additional OR staff is redundant. In fact, that’s far from the case. By reducing the scrubbed OR staff, we’re able to assign them to start the preparation for the next steps, and even the next surgery. That’s one of the contributors to reducing the operating room time and in turn increase OR throughput.”
Several factors are instrumental to standardization and ultimately improving process efficiency. Overall, it is not one efficiency measure that makes the difference. “It is the accumulation of multiple, often small, improvements that significantly impacts the efficiency gains.”
For example, OR tray reduction can significantly impact the OR process flow. “Most OR instrument trays have grown with multiple new instruments over the years. Do we really need all these instruments, or can we simply discard most of them? This was one of the first questions we asked ourselves,” says Prof. Corten.
The answer? After a couple of team meetings, Prof. Corten and his team were able to reduce his trays from 10 to only 3, including all regular instruments except for the power tools. “Today, my scrub nurse no longer has to search for any instrument. She just opens the tray and every single instrument in the tray will be used. No more, no less. No more losing time for instrument searching.”
“With the implementation of an efficient draping system, using the MedEnvision EsySuitTM, we’re able to reduce the preparation time significantly and already remove one of the variabilities from the equation. And while it’s faster, it’s also better ergonomically, limiting any high-risk poses for medical staff,” says Prof. Corten.
Next to efficient draping, Prof. Corten and his surgical team have also successfully implemented the use of a stable, hands-free retractor, the MedEnvision GripperTM.
We have found the GripperTM to be a highly impactful technology for introducing parallel processing during the surgery process. For instance, instead of holding the retractor for the surgeon, staff can be reallocated to other steps in the workflow. Simultaneously, the surgeon maintains a stable view of the surgical field and consequently conducts the procedure more swiftly.
Get access to the OR of Prof. Corten with the deferred live surgery application. Access here.
Measurements show what’s really happening in the operating room
Since the beginning of the collaboration with Prof. Corten, we’ve conducted hundreds of measurements in his operating room to gain a thorough understanding of the current processes and ways of working. To understand the process, we don’t need access to patient data or hospital records which ensures patient privacy and hospital compliance regulations are respected.
Conducting these measurements is the foundation for uncovering any variability in the intraoperative processes, identifying inconsistencies in the surgical process, and allowing for continuous improvement.
“Measurements give an excellent view into what’s happening in the operating room. They show the reality of how we work. They don’t lie. Sometimes, other surgeons are surprised to hear that I invite DEO into my OR to conduct measurements because there is a concern about being evaluated. But in the end, it’s not about me or my surgical technique. It’s about everything around the surgery, so I can keep focusing on the actual surgery and do the best job possible,” says Prof. Corten. “I want to improve my process. This allows me to conduct my surgery better, but also to introduce new technologies faster.”
Which kind of data is collected?
As Prof. Corten points out, the measurements we conduct in the operating room are not about evaluating people but about creating healthy working environments for the benefit of the medical staff and, ultimately, better patient experiences.
Now, what kind of data do we collect in Prof. Corten’s operating room to improve efficiency and ergonomics?
Generally, any data capturing and data generation are focused on:
- Process and resources
- Ergonomics
For process and resources, we typically collect information on workflows and timing (what is done when), staff allocation (who does what when), and resource usage like instrument trays, anesthesia type, implant size.
For the ergonomics measurements, on the other hand, the focus is looking at which movements and postures are performed by the team to determine if they are risky, done repetitively, and for how long.
Using our proprietary data analytics platform, DEO uses these measurements to quantify how standardized and consistent the OR process is and how well resources are utilized. Coupled with the outcome of ergonomics evaluation, this allows quick identification of improvement pathways.
However, there’s more at stake. With more than 50+ datapoints per surgery, we’re also able to identify potential for cost and waste reductions to benefit the hospital and larger healthcare community.
Prof. Corten adds, “In the OR, we sometimes have a gut feeling about what might improve the process but when we see the data—it’s very powerful to confirm these feelings with solid numbers. What’s even more helpful though is having the financial impact clearly mapped out in a business case when it comes to convincing hospital administration that one way or the other is better.”
With the 200+ surgeries we’ve measured in Prof. Corten’s OR, DEO has performed an activity-based cost analysis of the procedure to identify cost savings and build a business case for change implementation. By computing this as a unit cost, we can immediately show the financial impact by simulating any change(s) recommended.
Is operating room efficiency scalable?
The short answer is YES.
Prof. Corten performs surgery at other hospitals, in addition to ZOL, and has successfully implemented best practices to improve operating room efficiency there, too.
“Sure, the question of whether this solution is scalable to other hospitals has come up. And yes, it is scalable independent of the surgeon. Take the Anterior Approach as an example. It bears many advantages for the patient, but it’s a difficult approach to learn. The learning curve is steep. With a concept like the efficient surgery, we’re able to bring down the learning curve considerably because we reduce variability and make the procedure more consistent.”
Aside from Direct Anterior Hip Replacement, the operating room efficiency solution has also been used with other joint replacement procedures and can easily be applied to other specialties. The key performance metrics focusing on standardization and consistency informed by ergonomics and driving financial performance are applicable to any surgical process.
Do you want to know how we can help you get started? Schedule a 15-minute intro call. No strings attached.
PS. If you enjoy this content, you will definitely love the stuff we share on LinkedIn. Make sure you stay in the loop and follow our LinkedIn page.
Add Comment
You must be logged in to post a comment.