Operating room efficiency
In the current healthcare environment, improving the efficiency of operating rooms is critical to meeting the challenge of an influx of patients. But there is more at stake: employee well-being and financial viability.
Start by looking at surrounding factors
To improve and achieve a sustainable impact on operating room efficiency, we have found that it is critical to adopt a broad approach that balances all aspects influencing OR efficiency.
Our experience shows that focusing on factors surrounding surgery, including employee satisfaction, standardization, and simplification leads to increased surgery volume, improved total cost of surgery, and ultimately hospital cost savings (as shown in the visual below).
However, change must be implemented in a thoughtful, clearly defined manner to reduce the physical and mental impact on surgical teams.
This will foster a healthier work environment in the hospital and the OR with a sustainable workload that will improve the work-life balance among medical personnel and potentially increase patient satisfaction.
The good news is that there are plenty of opportunities to make this happen by leveraging a combination of digital technology, novel medical devices, best practices from the healthcare industry, and other manufacturing principles from automotive and aerospace.
What is operating room efficiency?
Efficiency in a surgical procedure is a measure of the time and effort required to perform the surgery. Hospitals often measure this to determine case volumes, room turnover times and rates, or patient anesthesia times.
Surgeons focus on OR efficiency to provide the best possible care to the largest number of patients, given the limited amount of time they can spend in the operating room.
They have found that a few key areas help improve their efficiency, including, but not limited to:
- Time management: properly scheduled day, respecting start times.
- Resource utilization: having the required materials and team members present in the OR.
- Minimal waste: reducing the amount of unused materials in the OR.
- Process optimization: having a well-coordinated team during the surgical procedure.
While these goals have been accepted as beneficial, it may not be clear how to implement these efficiency drivers. As a result, longer working hours and an increased workload are forced to compensate for inefficiencies.
This “work harder” approach is unsustainable.
Efficiency is the ability to perform surgeries successfully, and with high quality with minimal waste, expense, and effort, ultimately leading to optimization of OR time, cost savings, improved turnover times, and more.
How do you measure operating room efficiency?
Critical to operating room efficiency is adopting a broader mindset that expands the scope beyond surgical time alone.
Our experience shows that opportunities for improvement are often found in the setup and breakdown of the operating room.
Expanding the definition of what is involved in a surgical procedure to encompass the surgical team and the hospital system allows broader factors to be considered and, in turn, more opportunities for measurable and material improvement in efficiency.
Now, what do we specifically look at to measure OR efficiency?
How can we achieve comprehensive insights into what is happening in the operating room before, during, and after surgery to uncover where the opportunities for improvement lie?
Take a look at the Operating Room Efficiency Platform: Get the steps to getting started
Look at the operating room performance metrics
With our software and data analytics model, we measure the processes in the operating room to ensure a smooth flow. To quantify the process efficiency, we use a set of performance metrics.
Some of these metrics include standardization, OR occupation rate, turnover time, allocation, and utilization of human and material resources.
But there is more. Considering surrounding factors is just as important. In this case, it includes quantifying the fatigue that medical staff members experience during the OR process.
This is done through an ergonomic evaluation and scoring system also called the DEO ErgoScoreTM.
Together, these primary elements of operating efficiency and ergonomics are measured and quantified to gain critical insights into financial performance and staff well-being, with a focus on physical and mental fatigue.
As-is insights and improvement opportunities
Upon data generation, a detailed report typically follows, accounting for the operating room performance metrics of the as-is situation. Where relevant, the report also includes recommendations for efficiency, ergonomics, and financial performance improvements.
Examples of improvements and best practices
Such improvement opportunities vary and depend on the local situation of the hospital but may include changes like the ones mentioned in the list below:
- Optimization of flows in the operating room process
- Parallelization of processes to reduce turnaround times
- Implementation of efficient draping
- Better allocation of human resources for improved ergonomics
- Reduction of instrument trays
- Removal of process waste
The list continues and is highly dependent on the findings from the as-is data.
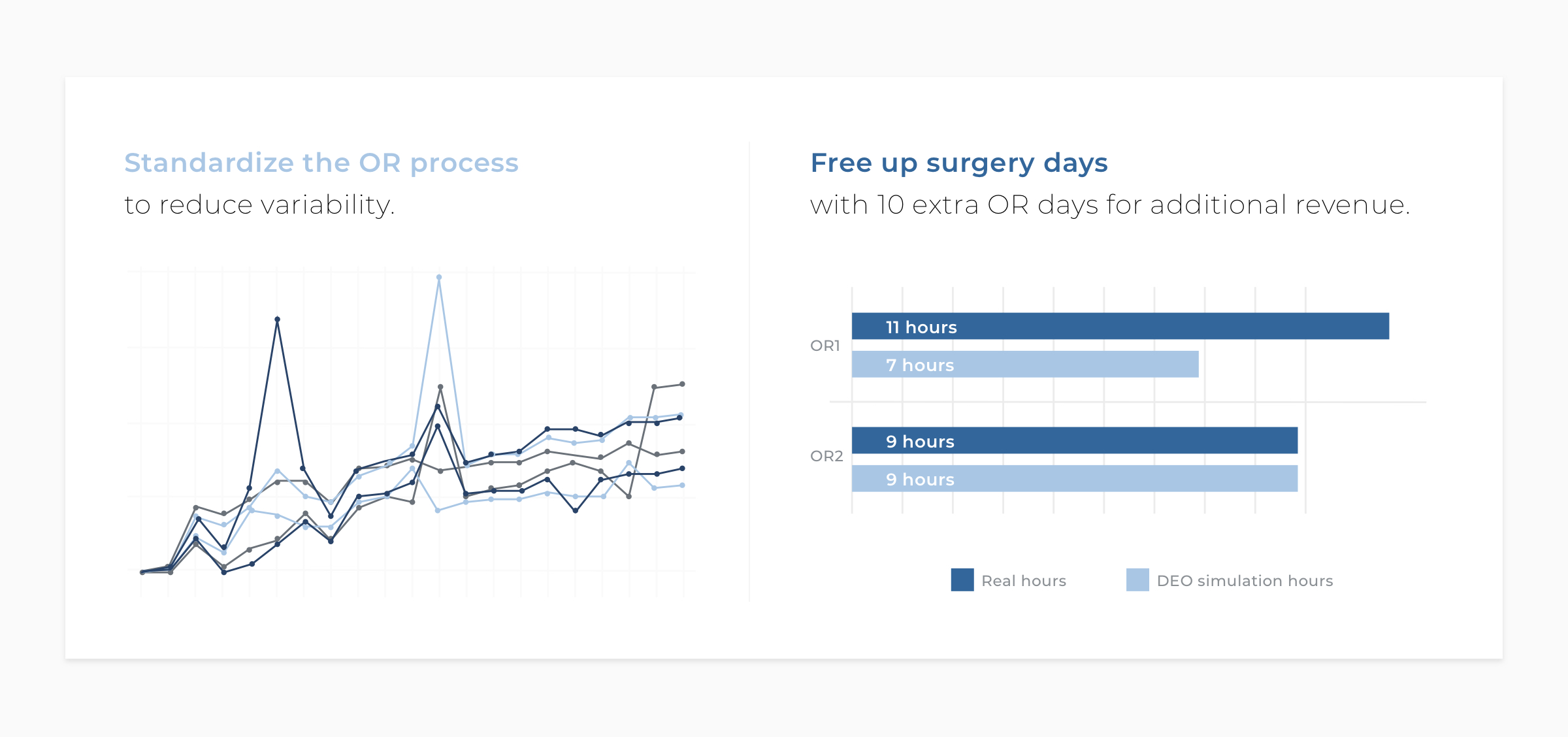
Simulated impact prediction and business case
Along with these insights and improvement opportunities, follow simulated impact predictions as well as argumentation why specific changes should be put first.
Together, this input makes up a proposed change roadmap for how to improve operating room efficiency and a business case containing a financial return on investment analysis to ensure hospitals get buy-in from all teams; surgeons, care teams, and hospital management.
Working smarter, not harder
In the end, operating room efficiency is a matter of improving processes and the working environment for surgeons and care teams, ensuring a smooth process that makes their job easier. Patient satisfaction and patient safety are naturally critical aspects, too.
It is about working smarter, not harder, alleviating the fatigue among medical staff, and improving job satisfaction.
When done right, the impact of improving operating room efficiency goes far beyond the actual operating room to also impact surrounding factors, budgets, cost savings, and ultimately increasing revenue.
Do you want to know how we can help you get started? Schedule a 15-minute intro call. No strings attached.
PS. If you enjoy this content, you will definitely love the stuff we share on LinkedIn. Make sure you stay in the loop and follow our LinkedIn page.
Add Comment
You must be logged in to post a comment.